Seven Tips to Protect the Arms, Knees and Careers of Young Catchers
There is a great demand for willing and talented catchers, and many great demands are placed especially on the shoulders, elbows, and knees of those who toil behind the plate.
From bullpen warm-ups to bunt defense to gunning out runners at second or third, catchers are a focal point of both practices and games.
All while doing the routine return throwing of the ball to the pitcher with most of this work done in the squat position with foul balls coming right at them.
In all, no player makes more total throws than a catcher.
Yes, the majority of those are fairly easy tosses back to the pitcher.
However, there are those harder pick-offs or throws to catch steals that only add to the cumulative stress.
And when pitchers get tired, they get replaced- unlike the catcher who tends to stay out there even for both ends of a doubleheader.
While there are pitch count limits and required rest days for pitchers, the only such formal guidelines placed on catchers are by Little League Baseball which mandates that any player who throws more than 41 pitches in a game cannot move to catcher in the same game.
So what other guidelines can help protect the overall health and longevity of catchers?
1. Have catchers alternate standing and being in the squat position with return tosses to the pitcher.
- Throwing from the squat is quicker and looks pretty cool, but the lack of lower body involvement in the throw places more stress on the shoulder. Coming out of the squat not only gets the legs involved in the throw but also reduces lower leg cramping.
2. Have catchers sit on a bucket for practice and bullpen sessions- allows them to give a consistent target while putting less deep squat-induced pressure on the lower legs. The "knee saver" products are designed in theory to similarly reduce deep knee bending in the squat position.
3. Try to limit unnecessary throwing during practices or bullpen sessions. Let catchers roll balls back or drop them in a bucket- less throwing means less overall stress and likely better throws when they matter.
4. Have a regular rotation of catchers. While inning counts or throw counts like for pitchers do not exist, monitor catchers for signs of fatigue such as slower to come out of squat, weaker throws back to pitchers or to bases, and giving a lower target due to shoulder fatigue. Better even to plan ahead with catcher substitutions rather than waiting for more obvious signs of overload.
5. Select sensible alternate positions- first base is attractive as there is a limited throw demand which then allows some arm rest, and also takes advantage of the fact that most catchers are taller and used to providing good targets for balls coming at them.
6. Caution with the pitcher-catcher combination that results in too many throws and increases the risk of injury.
7. Limit seasonal or annual arm overuse. Catchers playing for more than one team or not taking at least 2-3 months a year off from throwing are at higher risk of shoulder or elbow injuries.
Dealing with Detours- Lessons Learned as a Sports Medicine Physician
I have become more comfortable dealing with detours
Detours are going to happen.
We like to live in the ideal world where performance and recovery both travel a straight line ahead without and obstacles or set-backs. After carefully evaluating a situation, we thoughtfully construct a comprehensive plan, then look to execute it with frank precision.
Then reality kicks in, and the detours begin.
When I was asked to speak on behalf of friend and colleague Benjamin Strack, PhD on his installation as 2017 President of the Orange County Psychological Association, I shared insights that have been taught as part of the team behind the team learning from our best teachers- our patients and their families.
My focus was on Dealing with Detours.
Let’s be real.
Our athletes certainly also do not like to admit that detours occur.
How many athletes when asked about the start of season are going to tell you anything other than they're going to have an awesome time, the youngsters are going to come through, the opponents aren’t that tough, and big accomplishments on the horizon.
Does anyone ever say that they're going to anticipate obstacles, team dissension, untimely injuries, more talented and prepared opponents, bad losses and maybe even firings?
Detours come in the crucible of athletics that often place unique demands on young athletes.
While some athletes can handle detours without the blink of an eye, others will suffer from anxiety, depression, and other challenging coping behaviors.
Those of us who serve as the team behind the team are charged with the task of helping build a supportive culture focus on big picture outcomes such as success in sport translating to success in life, building healthy habits, and yes, navigating those detours.
Our presence as a sports medicine team is based on reacting to detours.
Just like no one athlete can emerge victorious to win all by him or herself, no good sports medicine effort is a solo performance. It is the ultimate function of a team that will often lead to the best possible outcomes.
Building the team behind the team and our relationships with athletes is a dynamic process.
The process starts with being available and that might be nothing more than hanging out at a practice, chasing volleyballs before gold-medal match, or helping fold towels between points. Those menial tasks are often the pathway to a higher level of engagement.
That availability also means being dealing with atypical situations at atypical times (before 9 AM and after 5 PM for certain) in atypical venues (on fields, over the phone).
No matter your level of availability to the team and athlete, you must keep your eye on the goal.
Developing trust that contributes to the ultimate short-term and long-term health of each individual patient.
This takes building a relationship.
When meeting with “the athlete” I attempt to separate the person from the the athlete identity. I may also separate from my team physician role- first and foremost, my priority is to be the medical provider for the athlete, above any team or group commitments.
Before asking about sports, I want to know what is going on in the life of the athlete: school, grades, outside jobs, family and friends, changes, substance use, sleep, appetite.
Once I get to know someone's goals, fears, and what truly is important in their life, then I feel I can make a greater impact with them. It often takes listening to the kid, independently from the parent, to meet these goals.
Be alert for transitions such as end of eligibility/career, injury, new team, new coaches, higher level of participation (intensive, summer camp, showcase).
Remember to emphasize confidentiality. Teenagers especially are quick to shy away from anything that will cause embarrassment or public scrutiny. They may Instagram multiple things about their life, but then can hide behind a wall of silence when they feel necessary.
When I eventually get to the sports thing, I ask about:
- Demands of the sport- time, intensity, and level
- Team Dynamics
- Multiple coaches and teams
- Flux of rosters, positions, starting spots
- Travel
- Financial/time commitment
- Perceived role
- Perceived voice
If you don't know exactly when an athlete does with the demands of their activity ask them. If they won't tell you then Google or YouTube it.
If there's been an injury, ask how the athlete is dealing with the new found free time away from sport demands.
Some find it liberating...don't be surprised.
Some don't miss their sport.
This leads into one big thing I have learned- don’t assume anything. Let me repeat that. Don't assume anything.
Believe in the art of negotiation. Our job is to advise and offer suggestions not unilaterally dictate a treatment plan. Amazing how sufficient discussion leads to the best answers, and often the athlete is the one coming up with the best answer.
Be ready to be pummeled for specifics- "what exactly can I do"? This can be painstaking but is absolutely necessary.
Allow exit strategies.
The ultimate best outcome of your professional involvement may not be wins or titles- it very well may not even be a return to sport.
Sometime a preconceived detour is actually a path towards something more rewarding.
Offer to take the hit for the athlete- if decision not to play, put all the blame on the medical team.
Give athletes the opportunity select how they want to mourn an injury or decision to retire. Some will totally distance themselves from the sport or team, while others want to have an active role. Help them in this choice
Don't feel the need to be a hero or go solo. Feel free to share the burden of difficult cases.
Always keep common themes and consistent messaging with athletes, families and other professionals.
Respect the hard work, past efforts, goals, dreams and commitment of the athlete and their schedule, but don't make decisions strictly based on the next big event.
Even if it's the Olympics.
Develop rapport before dropping bombs
Focus initially on performance enhancement. No kid will shy away from wanting to get better. Once you've built their trust and rapport, then you can delve into more of the sensitive emotional or behavior issues.
Learn to deal with uncertainty, with taking appropriately aggressive decisions that may work, or may run into those detours.
When confronted with setbacks or plateaus in recovery, continue to encourage the athlete. Try to limit conveying disappointment.
Finally, never wondering how to do something better, to keep learning, to keep finding more people to add to the team and help negotiate those detours.
Boarding, Biking and Skiing- Tips to Reduce Injury Risk
Skateboarding, BMX biking, snowboarding, skiing, and mountain biking are all sports practiced by dedicated athletes who put time and attention into bettering their tricks, handling, and overall skill. These athletes deserve credit for their abilities- and also should follow some basic recommendations to prevent injury and spending unwanted time away from the skate park or trails.
Do helmets actually prevent injury? How can I tell that a helmet is properly fitted?
Personal experience backed by multiple studies proves that helmets do prevent injury. For example, helmeted cyclists are 88% less likely to suffer a brain injury during a crash.
Every time some one gets on a vehicle with wheels (skateboard, scooter, rollerblades, and bicycle) or a snowboard, there should be a helmet on the head. A helmet hanging off the handlebars or kept in the garage is doing absolutely no good.
Helmets may not look cool, but a shaved head and scars from an accident look less cool.
Now, to be fully accurate, there are some limitations to helmets.
No helmet is 100% protective- they are designed more to reduce skull fractures than concussions.
Wearing a helmet does not give license to be more daring- make sure you read this a few times for emphasis.
A improperly fit helmet can reduce vision (which may increase, not decrease injury risk).
So, wear those helmets, understand limitations, and make sure they fit!
PROPER HELMET FITTING TIPS
- The helmet should sit level, covering the forehead in front with the strap adjusters fitting right under the ears and straps lying flat against the head; not hanging loose, curling out, or being twisted.
- Test for proper tightness by being able to put only one finger between the straps and chin and if helmet can be rocked from side to side, tighten straps.
- The helmet should rock slightly forward and backward, but tighten straps if it can be moved up off the forehead or down near the eyebrows.
- Add-on stickers and paint can personalize the helmet, but often void helmet warranties. Buy only helmets with CPSC, ASTM, or Snell stickers certifying safety standards.
- Multi-sport helmets should carry stickers certifying each sport- look for this sticker on the helmet, do not trust sales information or pictures on the box.
What is the scoop on wrist guards, elbow pads, knee pads and other protective pads and guards?
Many younger athletes do not like to wear pads, "they get in the way, get too hot, and they are not very attractive."
They do work, and work quite well in preventing broken bones, sprains, and road rash from falls or missed stunts. Experience has shown that wrist guards can greatly reduce the risk of forearm fractures due to falls from skateboards or snowboards.
Most people would prefer wearing protective pads and guards to wearing a plaster cast for 4-8 weeks.
A final statement: always know where you are going and be honest with your limits
- A common recipe for disaster is to barrel down an unknown trail unaware of obstacles or drop-offs that lie ahead. Taking the time to preview the course or to ride the pipe a few times at slow speed before trying tricks at full throttle can increase confidence and lower the risk of an unanticipated fall.
- Be aware of obstacles (rocks, trees, stairs, cars, and people) who might get in your away- always look forward 20-30 yards to anticipate any potential danger and to give time to make adjustments before an accidental impact.
- Be aware of your own skills- your strengths and weaknesses- and take into account your limits before deciding to do a particular course or maneuver. Do not be pressured by friends or your ego, if you do not feel comfortable riding the black diamond snowboarding run, do not do it. Have fun and build your skills at a run better suited for your abilities.
- Fatigue is also a major factor in injuries- many people decide to go out for one more run at the end of a long day, and that run ends up truly becoming the last one. Most authorities recommend stopping at the first signs of fatigue before judgment, endurance, and muscle strength become too low to prevent falls and serious injuries.
Dr. Koutures Co-Authors American Academy of Pediatrics Report on Martial Arts Safety
NEW AMERICAN ACADEMY OF PEDIATRICS REPORT ENCOURAGES SAFER PARTICIPATION IN MARTIAL ARTS
Nation’s pediatricians offer guidance on injury risks among various forms of martial arts, including mixed martial arts
Karate, taekwondo, judo and other martial arts can boost fitness, motor skills and emotional development for the estimated 6.5 million youth participants in the United States. But these increasingly popular activities also come with injury risks, which are strikingly higher for some techniques and movements within various disciplines.
A clinical report from the American Academy of Pediatrics (AAP) in the December 2016 journal Pediatrics, “Youth Participation and Injury Risk in Martial Arts” (published online Nov. 28), promotes safer participation in martial arts by guiding families to choose non-contact forms of martial arts that provide health benefits but lower risks of serious injury.
"There are so many different types of martial arts for families to consider and enjoy, but such a difference in injury risk between the different non-contact and sparring forms,” said author Chris Koutures, MD, FAAP, a member of the AAP Executive Committee on Sports Medicine and Fitness. “We hope that this report will enable pediatricians to help families select the most appropriate options for their child and realize how strongly certain practices and rules can impact a participant’s safety.”
Most martial arts injuries, such as bruises and sprains, are not life-threatening. But more serious injuries such as neck trauma, concussions and fractures do occur, especially during free sparring in competitions. Injury rates vary from 41 to 133 injuries for every 1,000 athletic exposures, depending on the form of martial art. Protective equipment such as soft helmets and mouth and face guards are not proven to prevent concussions and may provide a false sense of safety, according to the AAP.
The AAP recommends martial arts competition and contact-based training be delayed until children and adolescents demonstrate adequate physical and emotional maturity. The AAP calls for the elimination of certain rules, such awarding extra points during tournaments for kicks to the head, a rule recently enacted in taekwando, that can have particular impact on concussion rates.
The AAP strongly discourages youth participation in practices common in mixed martial arts (MMA) such as direct blows to the head, repetitive head thrusts to the floor and choking movements, which can dramatically increase risk of concussion, suffocation, spine damage, arterial ruptures or other head and neck injury. The AAP also cautions against excessive media exposure to MMA contests, which can put children at risk of injury if they imitate what they see.
Seven Practical Observations on Dealing with Shin Pain in Athletes
After seeing plenty of shin pain in ballet Nutcracker performers , Olympic Volleyball players and various other athletic activities , here are 7 practical clinical observations to help assess and treat this common problem.
1) Look above the shin
Landing from a jump with inadequate hip or buttock strength can lead to an inward collapse of the knee, placing abnormal rotational forces on the shin. Similar lack of upper leg control can lead to collapse of the foot arch in running, again causing increased stress on the shin. Any complete evaluation of shin pain should include some form of hip/buttock strength- my favorites include the single-leg squat, step-ups,or plie in 2nd position for dancers. Ideal alignment has kneecap directly under the hip and over the 2nd toe.
Plie in second position: note kneecap directly under hip and over 2nd toe
2) Look immediately below the shin
Decreased ankle dorsiflexion (ability to move shin towards the foot or foot toward the shin)is yet another contributor to increased stress of the shin bones. Common causes include tight calf muscles or restricted movements between the tibia (shin bone) and the talus (first bone of the foot). Side-to-side dorsiflexion motion comparisons can help identify abnormalities.
3) Try to stand on toes or walk on the outside of the foot
If the calcaenous (heel bone) doesn’t move inward when standing on the toes, or if there is an inability to walk comfortably on the outside border of the foot, start thinking about restricted midfoot subtalar joint motion. Much like limited dorsiflexion, subtalar dysfunction transmits excessive forces to the shin region. Tarsal coalition is a fairly common and under-recognized form of subtalar restriction.
4) Never under appreciate the importance of the big toe
Amazing how restrictions within the small 1st metatarsophalangeal joint (aka big toe joint) can lead to big problems in the shin. Limited ability to raise the big toe off the ground toward the shin leads to either increased pressure on the outside of the foot or higher forces on the front of the shin during foot impact with the ground. Stretching of the flexor hallicus longus muscle that controls big toe motion can be life and career-saving.
5) Stressful causes of cramping calves
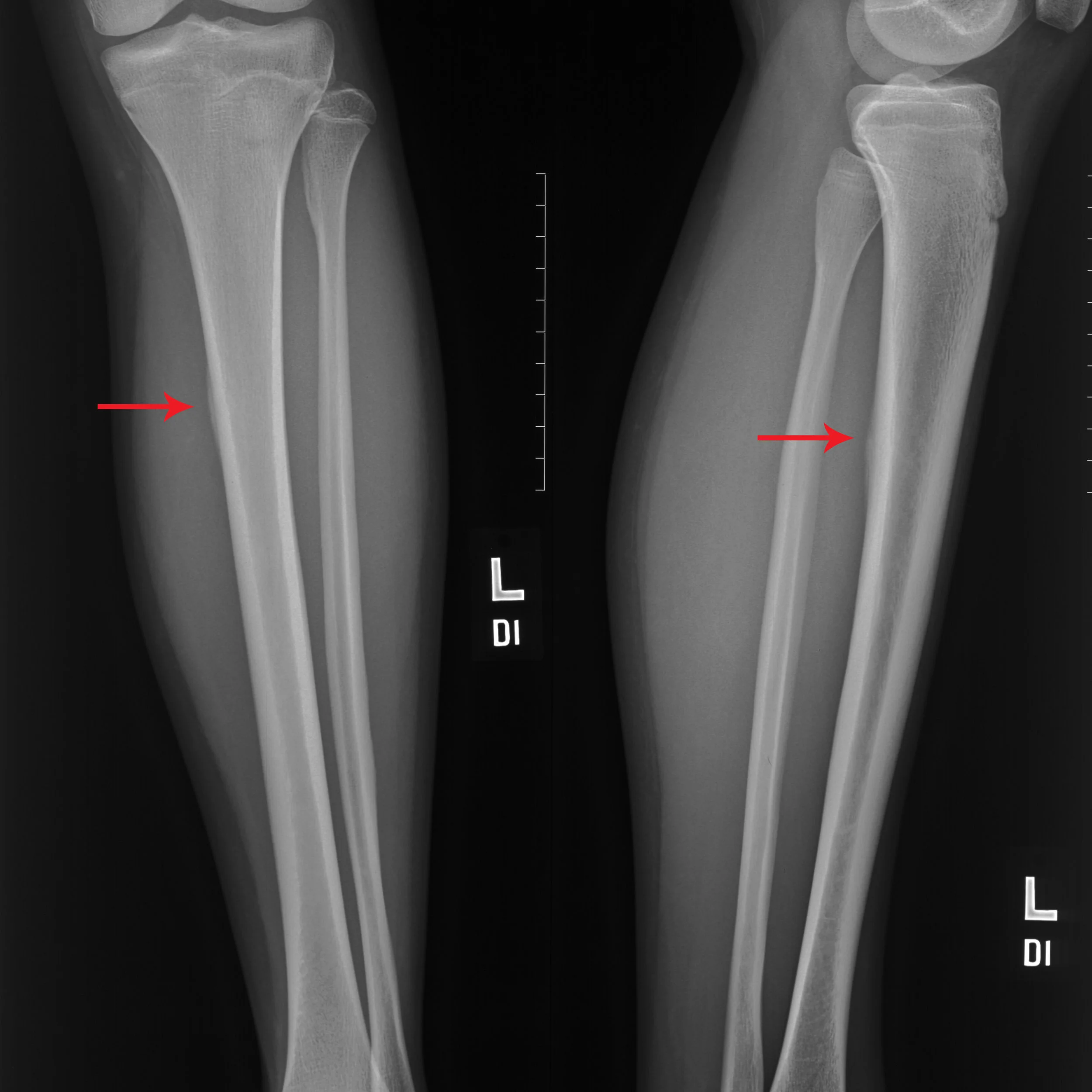
While most forms of generalized tightness or cramping in the calves are usually due to muscle fatigue and relative overuse, be more suspicious of cramps that can be pointed out by a finger tip and are located right next to the upper part of the tibia bone. Have found 2 recent cases of tibial stress reactions that presented with the primary concern of localized calf cramps.
6) How are the iron stores?
Some cases of long-standing or difficult to treat shin pain may be complicated by low ferritin (measure of iron stores in the body). More likely in females with heavier menstrual losses or those athletes and performers with restricted dietary iron intake. I will routinely order laboratory testing in my evaluation of challenging shin pain.
7) What are you wearing on your feet?
source:http://runhealthylifestyle.com/2016/08/25/careful-flip-flops-dangerous-summer-choice/
Practicing in Southern California, I often see patients who will select the best in athletic footwear, but then come into my office and routinely report wearing ill-fitting or poorly supportive shoes or sandals for non-athletic activities. I’ve learned that if you can twist a shoe or sandal like a rolled newspaper, then there isn’t much mid-foot support. Use of relatively inexpensive over-the-counter arch supports in daily use shoes can allow one to be both fashionable and functional, while leaving sandals for the pool or beach.
USA Volleyball Sports Medicine Experts Present at CHOC Children's Sports Cardiology Conference
The 2017 CHOC Children's Sports Cardiology Conference asks the question "What is the Role of the Cardiologist in the Sports Medicine Team?"
Our USA Volleyball Sports Medicine Team will be there to share our experience and provide our expert answers.
Several years ago, expert pediatric cardiologist Paul Grossfeld offered his services to USA Volleyball.
The results have been eye-opening and intriguing.
Focused elite athlete screening evaluations have not just provided insights for our players, but for all volleyball athletes and even other taller athletes participating in high level sport.
The process has not been without challenges.
Informing athletes of higher risk conditions and making decisions about career status and potential termination is never easy.
However, thanks to our on-going study, we have been able to contribute necessary data and experience to the conversation about screening and risk stratification in elite, taller athletes.
Our team looks forward to sharing this knowledge and extending our collaboration with important colleagues.
Pointing Out the Top 10 Pediatric Sports Musculoskeletal Injuries
The Top 10 Sports Musculoskeletal Sports Injury list is a ranking that I'm guessing most athletes don't want to make, and most parents don't want to miss.
How to best know if you belong on this list?
Trust your finger tips.
Speaking at the 2016 American Academy of Pediatrics National Convention and Exhibition, I was asked along with good friend and colleague Hank Chambers to share insight on identifying and managing the Top 10 Pediatric Sports Musculoskeletal Injuries with a Case-Based Review.
Our Top 10 aptly started at the top of the body (neck) and ran down to the bottom (foot/ankle) with several injuries in between.
We looked at:
- stingers
- shoulder pain
- elbow injuries
- wrist injuries
- low back pain
- hamstring avulsion injuries
- acute knee injuries
- shin pain
- ankle sprains
- heel pain in growing children.
Some were fairly serious and activity threatening, others were more of a nuisance.
A pretty diverse offering of injuries, so one would tend to think that there would be little that actually brings them together.
However, for those listening to the talk, they heard us mention a similar refrain over and over again.
The value of your finger tip.
In helping to determine a type of pain that merits medical attention in the first place, and helps sort out the particular diagnosis, the more localized the pain, the greater the potential concern.
For example,. if a child is reporting pain in the lower leg and uses a wave of the hand to indicate that the discomfort runs along the entire inner shin, then there is one level of concern.
However, if that same child takes the tip of their index finger and points directly and emphatically to a single spot on the inside of the shin bone, my concern is amped up several degrees.
While none of us have x-ray vision, that finding of finger-tip pain is a pretty good surrogate and does tend to correlate with a higher potential of a bone injury, be it a fracture, stress injury, or damage to a apophysis where a tendon attaches to a bone growth region.
So, no matter the body part, from elbow to wrist to foot or ankle, if any young athlete opts to use a finger tip to identify their pain, then use your finger tips to dial up your sports medicine specialist and seek out immediate and appropriate evaluation.
Wrestling: How to Keep Ideal Weight and Skin Health for Best Performance
How can I determine an appropriate wrestling weight? Is it OK to cut weight, and if so, how much is too much?
While there are often no easy answers or simple formulas to determine an appropriate wrestling weight, some standards can help the decision-making process:
- One can use a growth curve, which plots height and weight in comparison to age-matched individuals and also to past individual measures of height and weight. Can help determine if a desired weight "falls out" of the expected growth trajectory.
- The body mass index (BMI), which measures weight in regards to height, may help determine an appropriate body weight for a particular individual at a given age. Be aware that more muscular individuals may have an artificially high BMI, so this might not be the most accurate measurement in certain athletic individuals
- Another measure of body proportion called body fat percentage can help determine an appropriate wrestling weight though it historically has been used more to assess if an individual has cut too much weight. There are several methods for this measurement (calipers, bioelectric impedance, and water immersion) and a physician can help decide the most beneficial measurement, if needed, for a particular athlete. The California Interscholastic Federation now requires bioelectric impedance monitoring to determine appropriate pre-season weight class selections for high school wrestlers.
Once a wrestler is in season, authorities do not advocate more than a 2-3 pound drop in body weight when cutting weight for a match or meet. Good evidence tells us that a reduction greater than 2-3 pounds brings about dehydration and depletion of body energy sources that place the individual at greater risk for fatigue and injury. Many wrestlers know too well that after cutting a large amount of weight, they were not able to wrestle as effectively and many also report difficulties with concentration and schoolwork. This is particularly important in younger athletes who are going through key phases in physical growth and development.
When attempting to cut weight, use caution with any weight loss medication. Serious health issues can develop due to the use of these items, especially in growing athletes. If in doubt, consult with a sports medicine physician.
Frequent weight cycling (losing and gaining weight) can affect the immune system and make the athlete more at risk for respiratory illnesses and infections. This can be a major problem at the end of the winter season when many major meets take place.
How can we reduce common wrestling skin infections?
Due to close contact with mats and other athletes, wrestlers frequently contract skin diseases such as ring worm (aka tinea gladitorum), herpes, impetigo, and other infections. Not only are these a concern to the individual athlete, but they can easily spread to team members and opponents, thus officials routinely check the skin before large meets. To help prevent the disappointment of disqualification, the following recommendations may help:
- Wrestling mats should be cleansed with appropriate cleansing solution both before and after meets and practices.
- Wrestlers should shower after meets or competition and use a good anti-bacterial soap.
- Wrestlers should not share any personal care or grooming items (brushes, towels, razors, soaps, etc).
- In the ideal world, the athlete should shower before leaving the gym or school and have wrestling clothing cleansed on a daily basis.
- Coaches and parents should do frequent skin checks, and athletes should feel comfortable reporting any skin issues.
- Any athlete with skin concerns should be immediately removed from participation and evaluated by qualified medical personnel. This is particularly important early in the season to prevent spread to the entire team and a resultant season-long struggle with skin issues. Once appropriate treatment has begun, cover any areas of skin concern when returning to participation by using tape or a bandage which can do the trick in most cases.
What other wrestling safety tips do you have?
Good neck strengthening and stretching exercises can help prevent spine injuries, ask a sports medicine speciaist for good recommendations. Shoulder strengthening is also important for many of the holds and techniques used on the mat. Mouth guards are essential to reduce dental/mouth trauma so demand that wrestlers wear mouth protection for all practices and meets.
Dr. Koutures Quoted in: Girls More Prone to Sports Injuries- Here's Why
Team-Based Care and Cognitive Behavior Therapy Help Post Concussion Syndrome
Dr. Koutures Publishes on Dancers and Concussion in Journal of Physical Education, Recreation and Dance
Dancers are “artistic athletes.” They must possess the strength, agility, power and flexibility of any athlete and perform with perfect musicality and emotion, demonstrating the artistry of the dance. As an art form dance continues to push the physical boundaries of the human body, increasing the inherent risks to the dancers. Most injuries are readily acknowledged as a possible outcome of being a performing artist; however, the possibility of a concussion continues to receive little attention by leaders involved in dance education. The majority of dance and physical education instructors continue to be oblivious to the prevalence, diagnostic procedures, symptoms and appropriate reintegration into the dance environment after a concussion. Adapting the existing knowledge regarding concussion and sports, this article provides fundamental information to support the recovery and return to performance of a dancer with a concussion.
Click here to read the remainder of this important article to learn about:
- Evaluation of concussion symptoms and severity
- Treatment protocols for dancers
- Dancer reintegration after concussion
How Much Rest Right After a Concussion?
A 16 year-old running back suffers a direct blow to the head in a Friday night game. He immediately has a headache and dizziness and is removed from the game. He is sent home in the care of his parents after a discussion of particular signs and symptoms that would require emergency evaluation, and follow-up on Monday has been arranged with the his pediatrician.
In the meantime, what should he be able to do over the weekend?
Traditional post-concussion recommendations have focused on strict limitations in both cognitive and physical activity until resolution of concussion-related symptoms. The “cocoon treatment” where absolute avoidance of all stimulation, often carried out in a dark bedroom for several days, was one such initial recommendation.
More recent data suggests that over-aggressive reduction of cognitive and physical stimulation may actually prolong post-concussion recovery. Thomas et al in Pediatrics found that a strict 5 days of rest resulted in more daily reported symptom scores and slower symptom resolution versus 1-2 days of rest followed by stepwise return to activity. Zemek et al presented a paper at the 2016 Pediatric Academic Societies Meeting reporting that exercise within seven days of injury was associated with nearly half the rate of persistent post-concussive symptoms, or those that last beyond a month.
Striking a balance between overstimulation and understimulation is best done on an individual basis taking into account symptoms and patient preference. Allowing brief (initially 10-15 minute) intervals of activity such as light reading, listening to music, easy walking, or even texting can reduce feelings of isolation and foster recovery. Patients should focus on one activity at a time (no “multitasking”) and should immediately stop activities that result in worsening of symptoms. Regular medical follow-up evaluation can help determine further at-home activity recommendations and also guide return to learn and ultimate return to sport progression.
Sports Experts Answer Key Questions about Early Sport Specialization
I strongly recommend that parents, coaches, and other youth sport stakeholders review the clinical report Sports Specialization and Intensive Training in Young Athletes written by trusted colleagues with the American Academy of Pediatrics Council on Sports Medicine and Fitness led by good friend and passionate advocate Dr. Joel Brenner.
As a big fan of relevant question/practical answer format to best translate scientific studies to meet real-world challenges (see my Children and Sports Guide for example), was pleased to see common questions addressed and I will summarize their thoughtful responses below:
Does Specialization Lead to a Successful Performance and Career?
Most authorities agree that sports specialization, in general, leads to higher athletic “success,” but the optimal timing of specialization is only now becoming clearer. Studies have shown that Division 1 NCAA athletes are more likely to have played multiple sports in high school and that their first organized sport was different from their current one. Many examples exist of professional athletes who have learned skills that cross over to their sport by playing a variety of sports into high school and even college. There were 322 athletes invited to the 2015 National Football League Scouting Combine, 87% of whom played multiple sports in high school and 13% of whom only played football. Other studies in elite athletes have shown that intense training did not start until late adolescence and that these athletes played other sports before specializing. Reviews of studies of elite athlete specialization history revealed that, for the majority of sports, late specialization with early diversification is most likely to lead to elite status. In addition, athletes who engaged in sport-specific training at a young age had shorter athletic careers.
Are 10,000 Hours Needed to Succeed in Sports?
It has often been misquoted that to succeed, an athlete needs to have 10 000 hours of practice/competition over 10 years. The media have incorrectly extrapolated studies of chess players to a formula for sports success. Many examples exist of successful athletes who have <10 000 hours and others who have not succeeded despite having >10 000 hours of practice/competition. Other factors come into play besides sports exposure time. These may include physiologic construction (ie, a high jumper with elastic Achilles tendon) and genetics. For some athletes, elite status may be achieved with 10 000 hours of total deliberate play (child determines activity) and deliberate practice time (adult determines activity) in all sports combined but only 3000 hours of sport-specific training. Evidence is lacking that specialization before puberty is necessary to achieve elite status, and in fact, specialization before puberty is more likely to be detrimental.
When Is It Appropriate and Safe to Specialize?
Current evidence suggests that delaying sport specialization for the majority of sports until after puberty (late adolescence, ∼15 or 16 years of age) will minimize the risks and lead to a higher likelihood of athletic success.Only 0.3% of German athletes in Olympic sports selected at the youngest level were ranked internationally, and most elite athletes specialized in their primary sport later in life. Specialization can be divided into early versus late, with the inclusion of early diversification of multiple sports for those who specialize later. Early diversification allows the athlete to explore a variety of sports while growing physically, cognitively, and socially in a positive environment and developing intrinsic motivation. Young athletes can learn many important fundamental physical movement skills with early diversification that can then transfer over to their primary sport if they decide to specialize later. By learning these skills during their developing years through deliberate play (child directed activities), athletes will require less deliberate practice (adult directed activities) to acquire expertise in their chosen sport. Studies have also shown that deliberate play is crucial to normal development and attainment of elite status.Athletes in late adolescence have the cognitive, physical, social, emotional, and motor skills needed to invest into highly specialized training. They can understand the benefits and costs of intense focus on 1 sport and, just as importantly, are able to make an independent decision about investing in 1 sport.
What Are the Risks in Specializing Too Soon or at All?
Young athletes who specialize too soon are at risk of physical, emotional, and social problems. Specializing early with intense training can lead to overuse injuries, which can cause pain and temporary loss of playing time or may lead to early retirement from the sport. The risk of injury is multifactorial, including training volume, competitive level, and pubertal maturation stage. One study in high school athletes showed an increased risk of injury when the training volume exceeded 16 hours per week.. Another study determined that sports specialization was an independent risk factor for injury and that athletes who participated in organized sports compared with free play time in a ratio of >2:1 had an increased risk of an overuse injury. This same study found that young athletes who participated in more hours of organized sports per week than their age in years also had an increased risk of an overuse injury. Burnout, anxiety, depression, and attrition are increased in early specializers. Social isolation from peers who do not participate in the athlete’s sport and lack of being exposed to a variety of sports also are concerns. Restriction in exposure to a variety of sports can lead to the young athlete not experiencing a sport that he or she may truly enjoy, excel at playing, or want to participate in throughout his or her adult life. An additional concern is the risk of physical, emotional, and sexual abuse by the adults involved in the young athletes’ lives as a result of overdependence. Dietary and chemical manipulation are also possible. The combination of these adverse outcomes could lead to a decrease in lifelong physical activity.
Which Sports Require Early Specialization and Are Those Athletes at High Risk?
Figure skating, gymnastics, rhythmic gymnastics, and diving may require early specialization, because peak performance occurs before full physical maturation.However, it is not known whether the training required for such sports poses a risk for athletes’ long-term health and well-being. Studies in gymnasts and figure skaters found that their training did not affect pubertal growth and maturation or adult height. First menstrual period occurred later but within a normal range. However, other studies have shown that female athletes who participate in sports requiring early sports specialization are at higher risk of overuse injuries as well as bone stress injuries, disordered eating and menstrual irregularities.
How Much Training Is Adequate to Succeed Versus Too Much?
The exact amount of training needed to succeed has not been described. The threshold to avoid injuries, burnout, and attrition has not been elucidated. The possible rule of participating in fewer hours of organized sports per week than their age in years or restricting training to <16 hours per week to decrease the chance of injuries needs to be validated by other long-term studies.
Do Sports-Enhancement Programs Lead to Success?
Young athletes need to learn motor development skills, social skills, and psychological skills to succeed. No studies on sports-enhancement programs in youth that only teach sport technique or “conditioning” have shown a greater chance of success despite their increased time and financial investment.
What Are the Effects of Early College Recruitment?
Talented youth are starting to be ranked nationally as early as sixth grade. As colleges start to look at middle school and early high school athletes, more pressure is created for the athlete and parent to do everything possible to succeed. This situation may push athletes into playing year-round and possibly on multiple teams simultaneously to get more exposure and specializing in a single sport sooner for fear of missing their opportunity to impress a college coach. Given what is currently known about early sport specialization, this changing paradigm should be discouraged by society. The AAP, NCAA, pediatricians, parents, and other stakeholders should advocate banning national ranking of athletes and college recruitment before the athletes’ later high school years.
4 Points that Matter about Post-Concussion Return to Learn
Completely enjoyed learning from Brenda Eagen-Brown- one of the true passionate authorities on post-concussion return to learn, and wanted to share some key "take-away" points from her awesome presentation.
All pictures are from her slides, and comments afterward are mine.
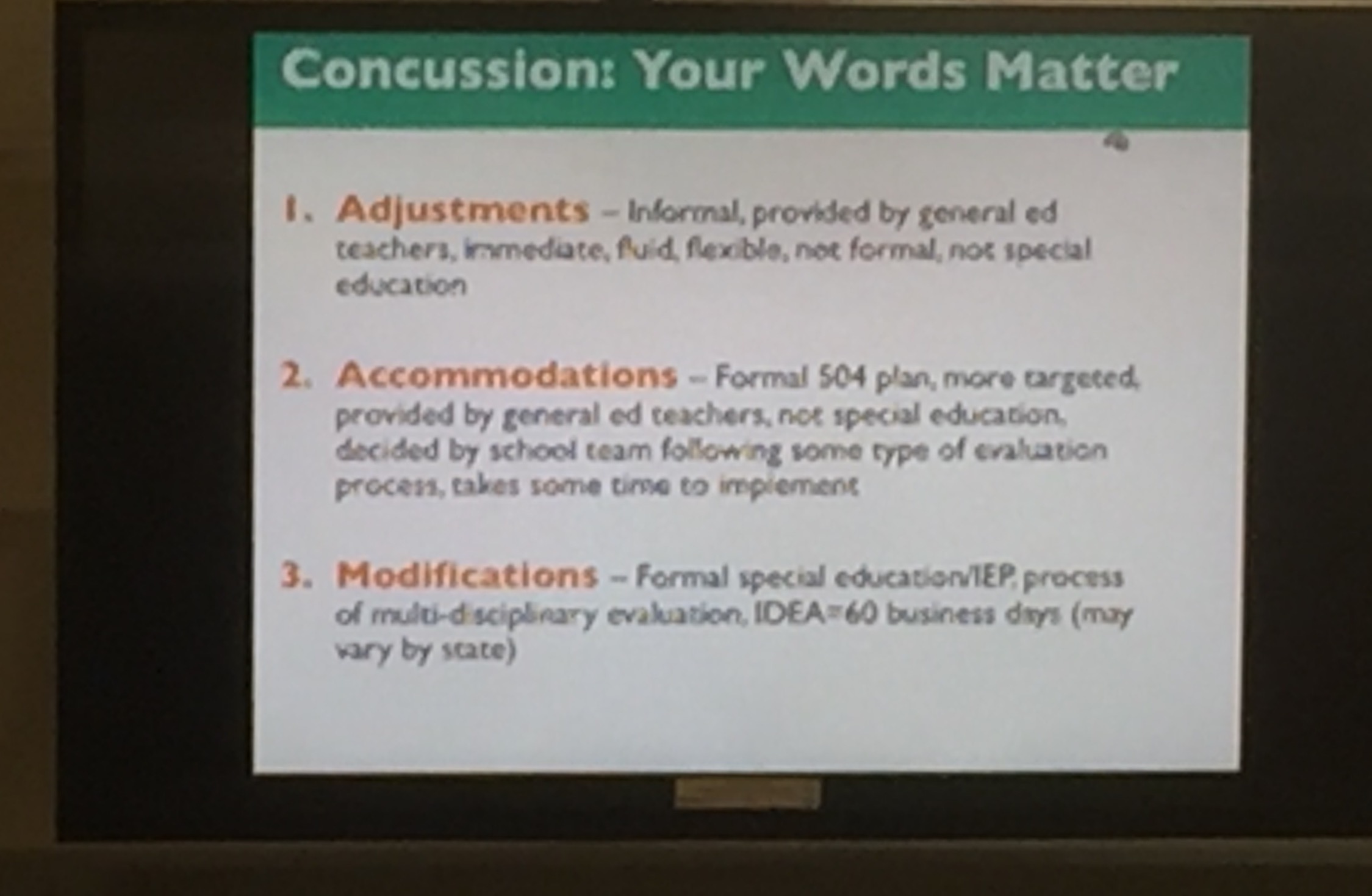
Make sure there is consistent agreement on terms describing what assistance students may receive after a concussion.
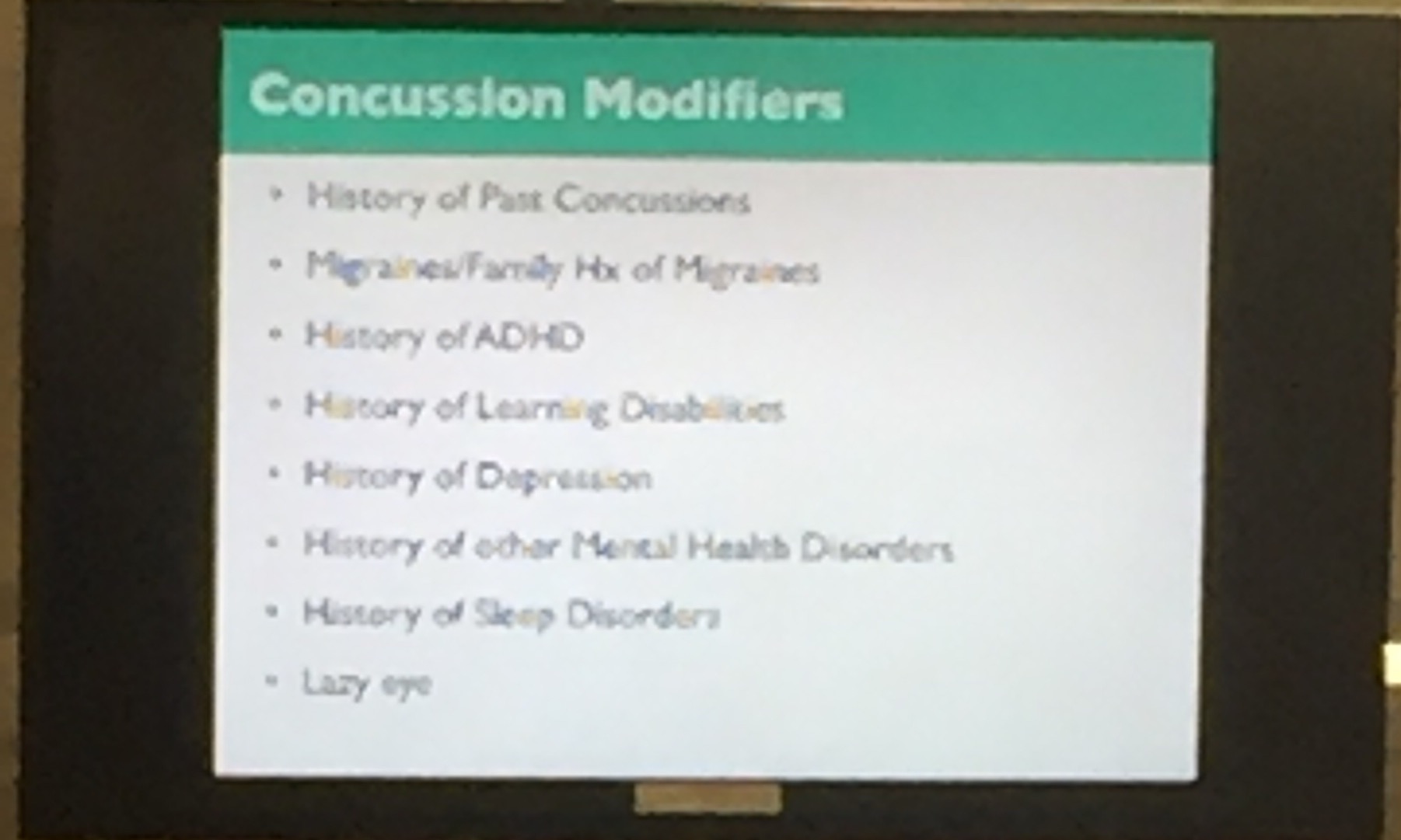
Absolutely essential to have all providers ask about these key historical aspects that can and often will impact concussion recovery. If a patient appears to have a more prolonged or difficult post-concussion course, very likely one or more of these items will be a factor. Don't hesitate to ask at multiple encounters as many patients won't initially offer or give sufficient details about pertinent past history.
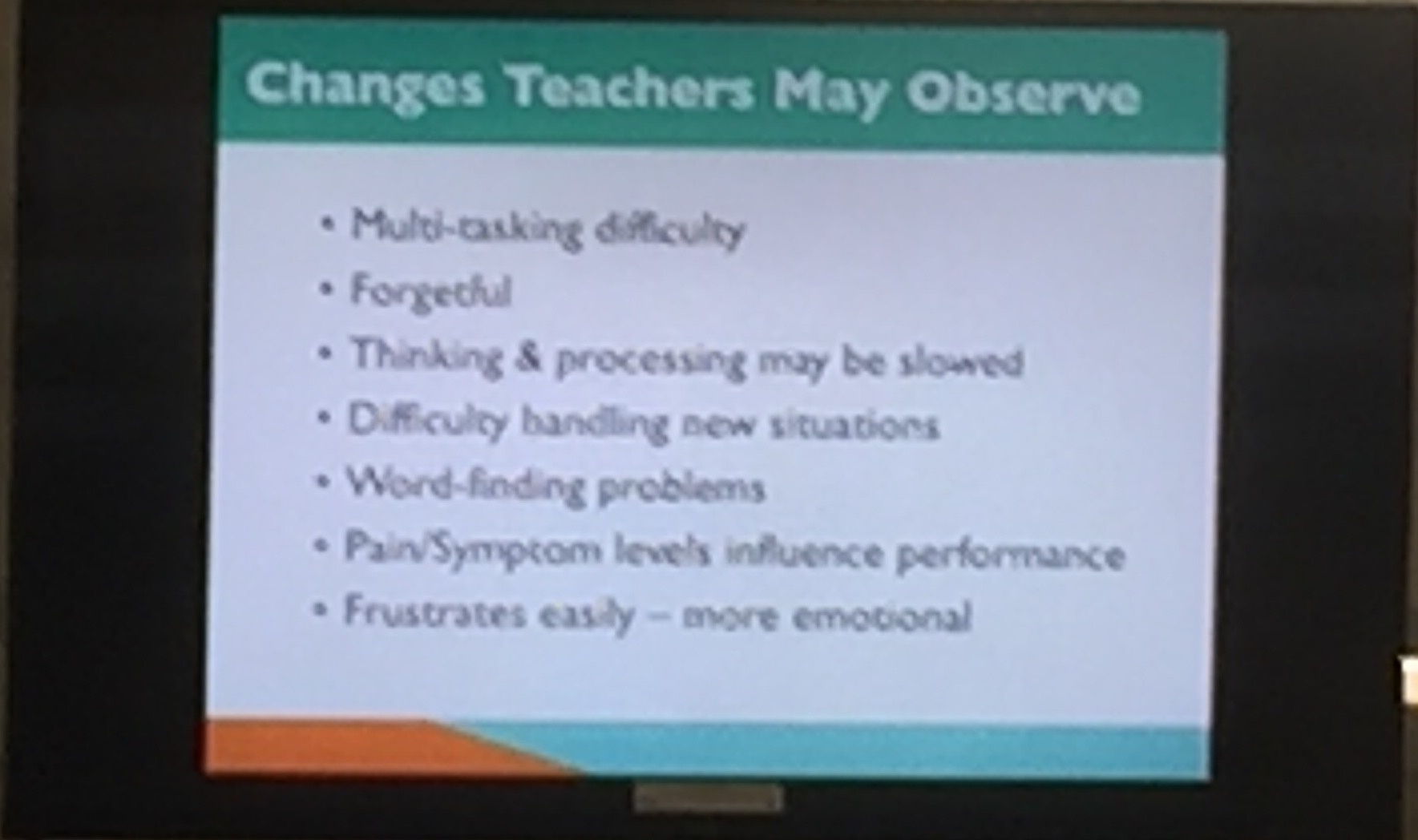
Great summery of changes that not only teachers should be assessing but also provide the framework for medical providers and families to address classroom difficulties. One of Brenda's key points- recall issues after concussion tend to be difficulties with information retrieval ("on the tip of my tongue") than true memory deficits.
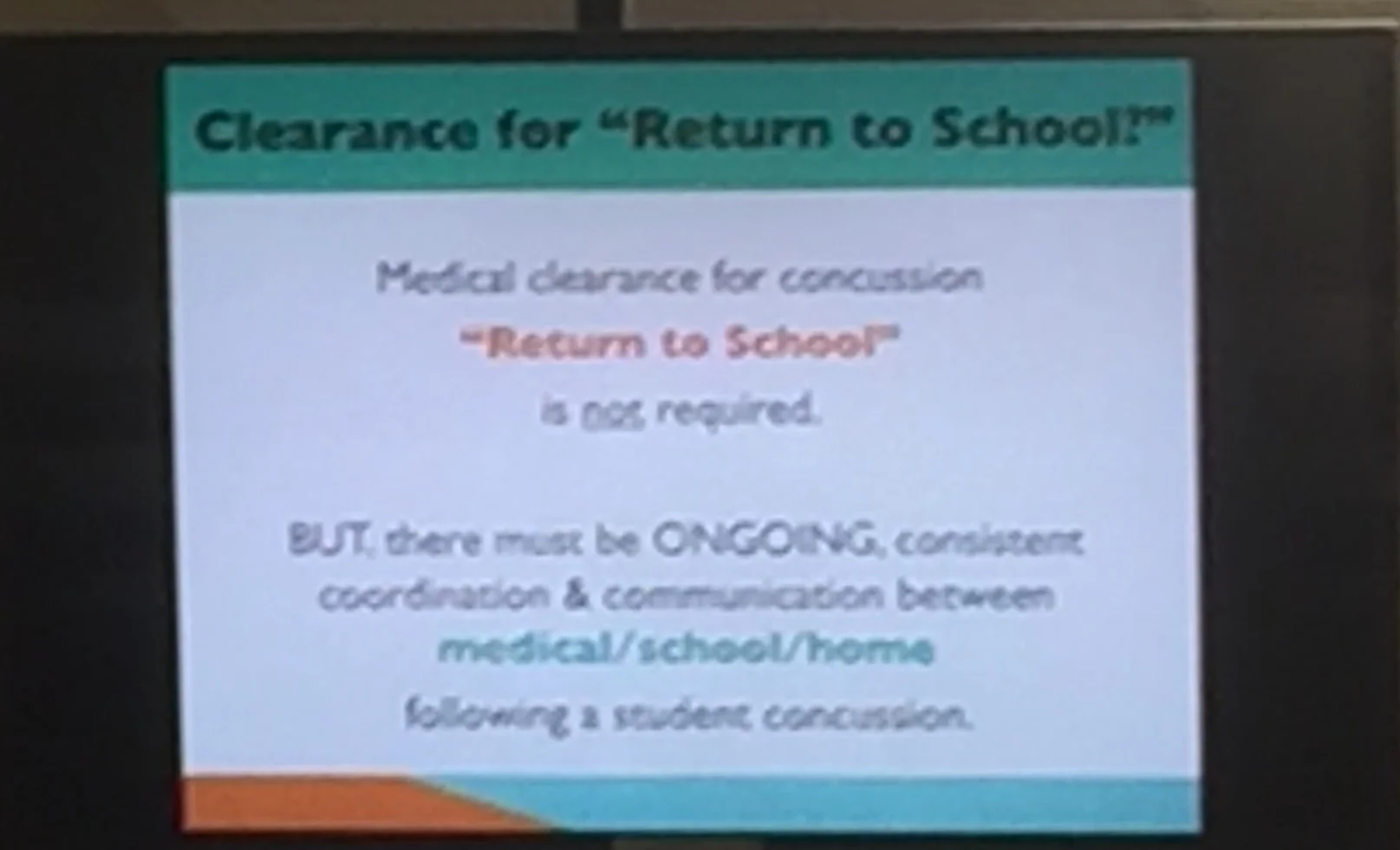
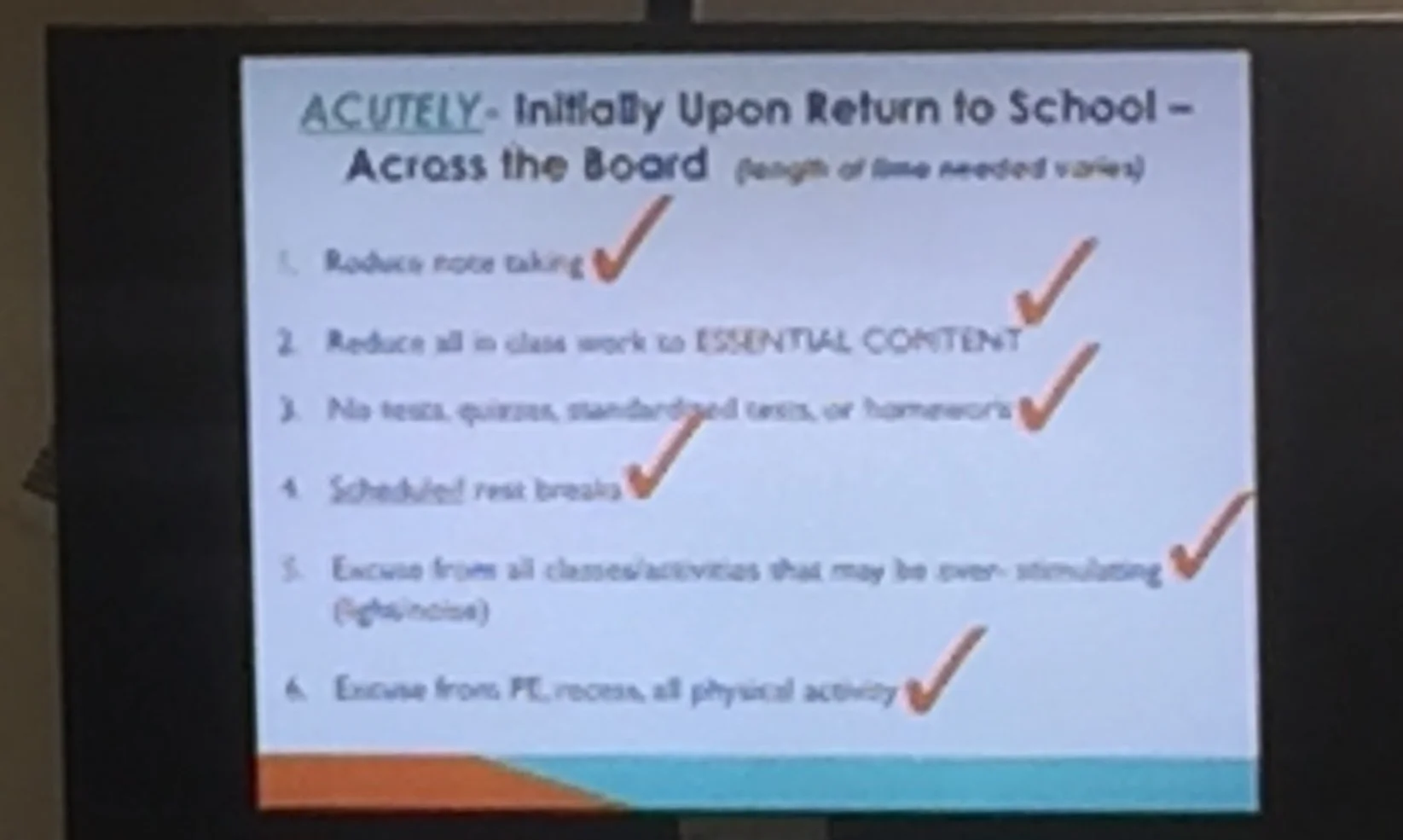
Many benefits to a standing protocol for initial return to learn that doesn't need medical clearance that immediately addresses student need. Extra emphasis on the scheduled rest breaks as waiting until symptoms erupt only slows the recovery process. These efforts attempt to reduce over-stimulation or emotional flooding that more readily occurs during post-concussion recovery as the brain's "filters" are not functioning properly.
Learn From the Team Physician to USA Volleyball Olympic Bronze Medalists
Congratulations to the 2016 Bronze Medalist USA Men's and Women's Olympic Volleyball Teams! Get the same expert sports medicine care that Olympic volleyball athletes received on the Road to Rio.
Book a visit with Dr. Koutures to discuss volleyball injuries or schedule him to speak to your team, coaching staff or families.
Some common topics he can address include:
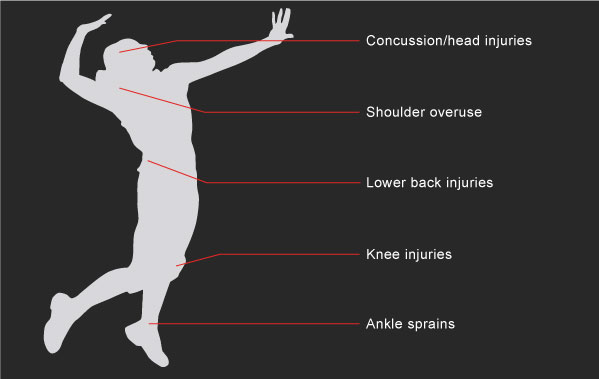
- How can overuse/overload volleyball injuries of the shoulder and knee be reduced or prevented?
- Improper shoulder or knee/lower leg mechanics can contribute to lower back injuries. Find out how proper swinging and landing techniques can protect not only shoulders and knees, but also the lower back.
- While volleyball is often considered to be a lower-risk sport for concussion, liberos are at particularly higher risk. Learn how to reduce risk and also how to respond to a potential concussed player on your team
- Taller volleyball players may have certain heart issues not commonly found in shorter athletes. Find out how the USA Volleyball National Teams screen their athletes and if your volleyball player would benefit from similar evaluation.
- Most shoulder injuries in volleyball players can be treated without surgery. Before agreeing to shoulder surgery, learn the techniques used by the USA National Volleyball Teams to avoid or put off the need for shoulder surgery.
- Should volleyball player wear ankle braces? Hear the pros and cons from a sports medicine specialist who has gathered opinions from elite volleyball players and fellow volleyball sports medicine expert colleagues.
Three Key Questions that can Reduce Overuse Injuries in Young Dancers
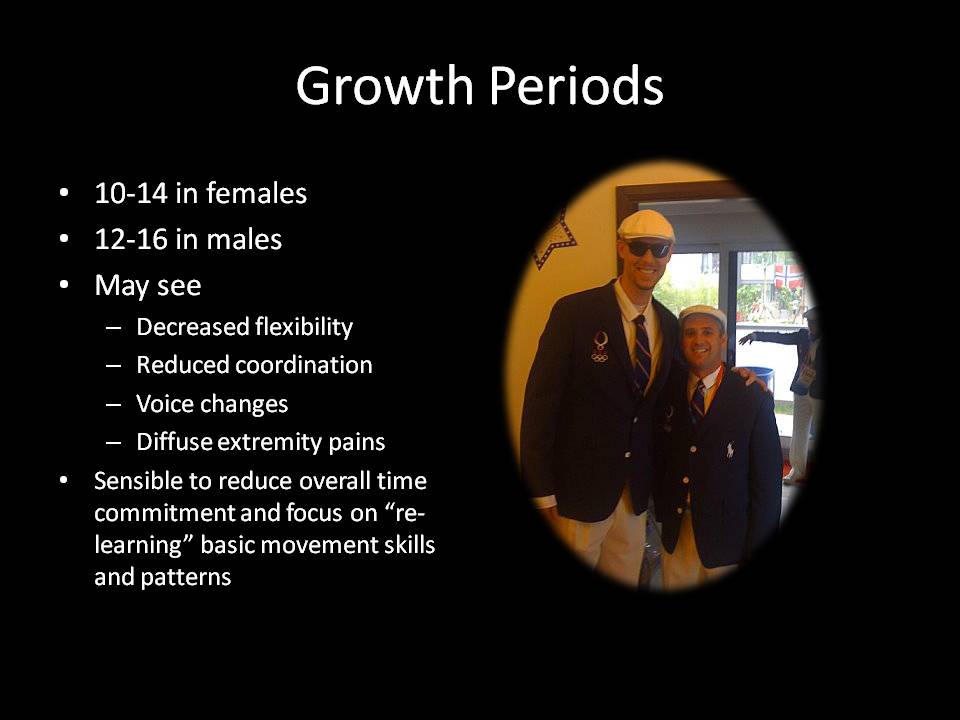
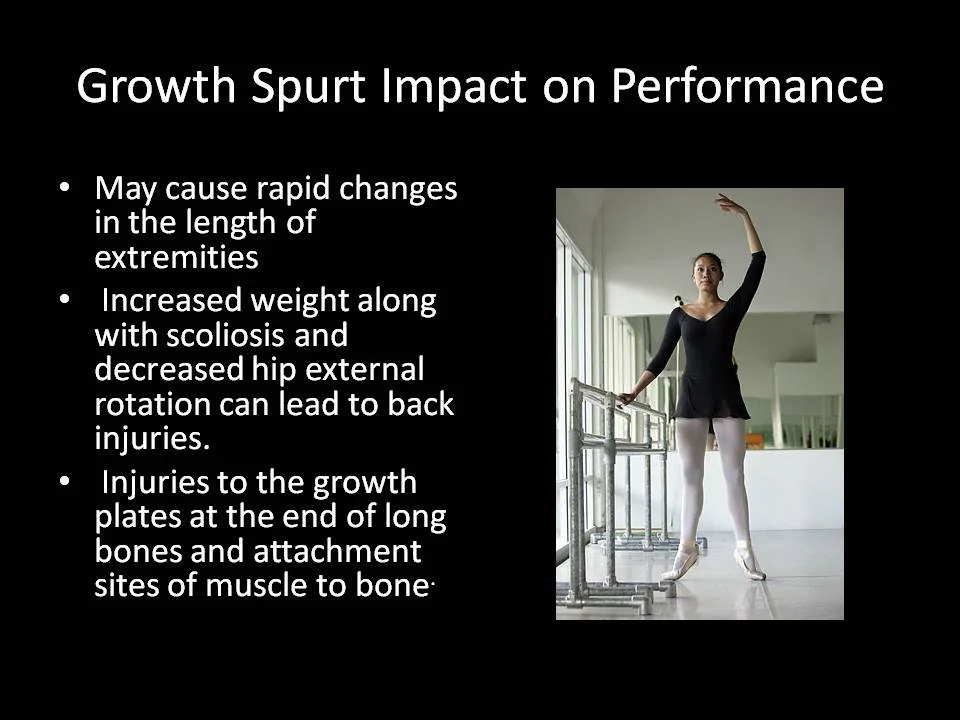
1. Am I going through a growth spurt?
Bottom Line: Longer arms and legs are harder to control without appropriate strength in the shoulder and hip areas. While many pre-teen and teenage dancers want to amp up dance commitments, growth periods are not the best time for adding more technically demanding routines. Stick to basic movements, build central strength, and once in better control, then more ready to step up the skill requirements.
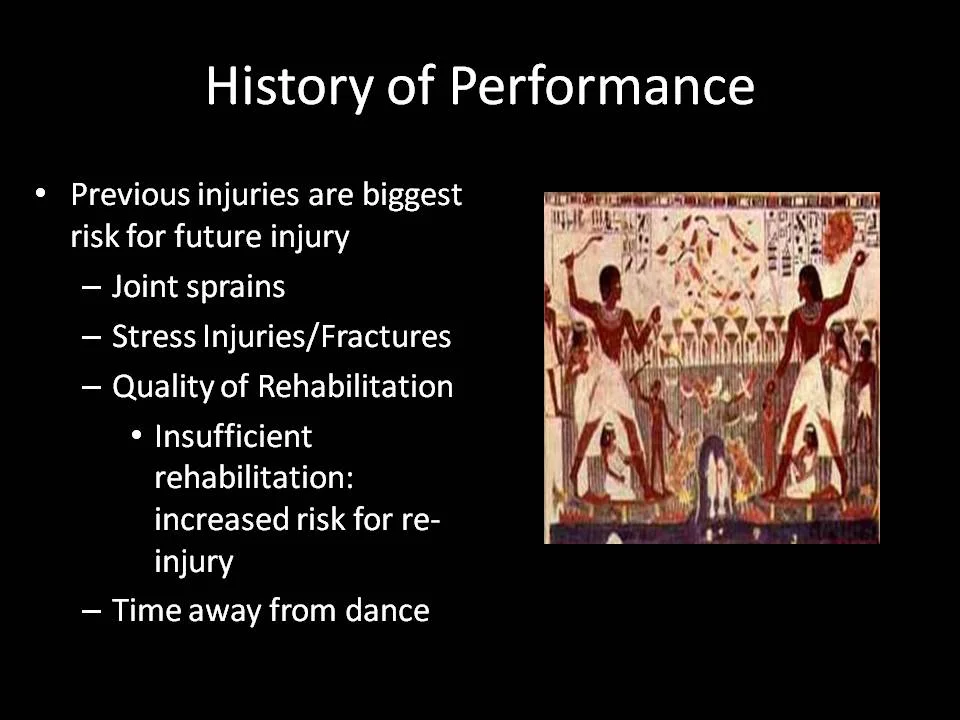
2. Am I still getting over a past injury?
Bottom Line: Trying to push through a past injury that hasn't fully healed is a recipe for future trouble. Better to take a step back, get proper medical care, and when more healthy, then push ahead with more classes and more intense routines.
3. How old am I?
Bottom Line: Absolutely the best evidence out there to reduce overuse injuries, and very easy to remember. If your age in years is lower than the number of hours of organized dance activities per week, your injury risk goes up in dramatic fashion.
Schedule Dr. Koutures to Speak to Your Soccer Club or Team
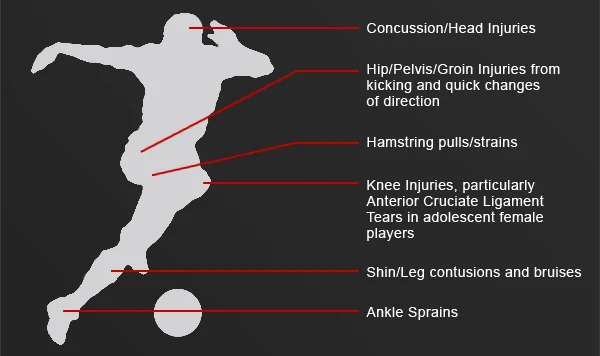
INJURY PREVENTION: SOCCER
With more and more kids and teens playing soccer, so comes the risk of injury. Today, players are suffering from head injuries, groin injuries, knee injuries, hamstring pulls and broken bones.
Schedule Dr. Koutures to come speak to your coaching staff or families!
Some common topics he can address include:
- How to interpret new US Soccer Heading Guidelines and put them into practice, and how to respond to a player who may have or has suffered a concussion.
- How to keep your players on the field and their knees in healthy playing condition. Anterior Cruciate Ligament (ACL) tears are all too common in soccer, especially in adolescent female players, but scientifically studied warm-up programs can reduce the risk.
- Playing in tournaments with multiple games over a short period of time? Learn how certain nutrition tips and the importance of adequate sleep can assist with recovery and contribute to better soccer performance.
- Soccer injury prevention tips from the pediatric sports medicine specialist who co-authored the American Academy of Pediatrics Policy Statement on Injuries in Youth Soccer.
To schedule a one hour session with Dr. Koutures for coaches and/or parents, click here or call 714-974-2220