Repetitive Ankle Sprains or Recurrent Ankle Swelling- Three Common Causes
When an athlete presents to me with concerns over multiple ankle sprains or on-going ankle swelling, what thoughts go through my mind?
- Inadequate Rehabilitation of Previous Ankle Injuries
- The number one risk factor for future ankle injury is under-rehabilitation of a past ankle injury.
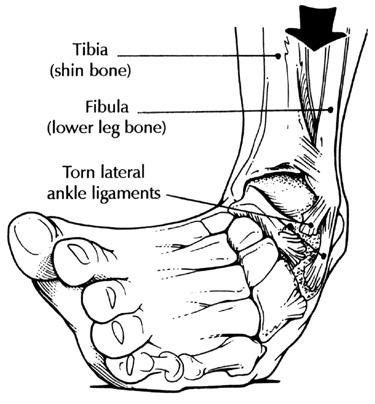
- Ankle sprains are defined as stretching or partial/complete tears of the ligaments that connect bones on the outside and inside of the ankle joint. The majority of ankle injuries are caused by rolling in of the foot (called an inversion ankle injury) and cause damage to the anterior talofibular and calcaneofibular ligaments on the outside of the ankle. Injuries with rolling out of the foot are less common and cause injury to the deltoid ligament on the inside of the ankle.
- The healing process with a damaged ligament leads to scar tissue formation at the site of the tear. Trying to come back too soon after an ankle sprain will limit the scar formation and predispose the ankle to future injury.
- Even with appropriate recovery time for scar formation, a sprained ligament is never completely as strong as prior to injury. Undertaking an appropriate rehabilitation program that builds up the strength and proper firing patterns of the peroneal muscles on the outside of the ankle can help compensate for the reduced ligament strength and reduce risk of later injury. Increasing strength of the muscle above the ankle, including the hip rotators, can also reduce the risk of future ankle problems.
- Underlying Structural Abnormalities such as Tarsal Coalition
- The ankle joint is defined as the "upside-down U shaped mortise space" between the tibia (shin bone), fibula (thin bone on outside of lower leg) and the talus (first bone of foot). Below this mortise ankle joint are the sub-talar joints which include connections between the heel bone (calcaneous), talus, navicular (bone on top of inside foot arch) and cuboid (bone on outside of foot).
- Abnormal bone or fibrous soft tissue bridges between these tarsal and sub-talar region bones can develop as part of on-going foot development or after an injury and can lead to restrictive motion of those sub-talar joints causing increased stress and higher risk of ankle sprains.
- What are physical exam findings that suggest tarsal coalition?
- Ask patient to walk with the feet turned in- they cannot turn feet in sufficiently to walk on the outside of the feet
- Ask the patient to stand on toes with heels raised- when viewed from behind, the heel bone will not turn in (invert) suggesting reduced subtalar motion
- Often these subtle physical exam findings are the best initial clues for discovering tarsal coalition
- X-ray examination may show osteophytes (extra bone) on the front aspect of the talar neck (white arrow below), a prominent lateral process of the calcaneous, and narrowing of the joints below the talus (black arrow below). In many cases, Magnetic Resonance Imaging (MRI) or CT Scan might be needed to better define the anatomy
- Osteochondral Lesions of the Talar Dome
- The top part of the talus bone (known as the dome) is covered by articular cartilage, and one or more ankle injuries can cause damage to the cartilage and underlying bone known as an osteochondral lesion.
- Osteochondral lesions are notorious for not appearing on initial x-rays taken at the time of injury. Don't be fooled or lulled into complacency with normal early x-rays and an ankle that isn't getting better.
- A classic presentation is the case of an ankle sprain which never fully recovers and results in chronic swelling of the ankle joint associated with clicking, catching, or locking sensations.
- Often, repeat x-rays taken weeks to months after the injury may reveal signs of an osteochondral lesion (black arrow) with separation, fragmentation, and irregularity seen at the talar dome. MRI might be used to better categorize the nature of the injury.
This blog post is not intended to diagnose or treat any ankle or other injury. If you have concerns over repetitive ankle injuries or recurrent ankle swelling, please contact me or your sports medicine specialist for a proper evaluation or treatment plan.