Exercise when Sick: Stop? Go? How to Reduce Risks?
Is it OK to exercise when sick? What symptoms should keep someone off the playing field?
When trying to decide if an athlete is too ill to participate in sports, I tend to ask the following questions:
- Is the athlete currently too ill to exercise?
- Will exercise make the athlete at-risk for more serious or longer-lasting illness?
- Is the athlete contagious to other members of the team or sport group?
Study and experience tells us that a fever over 100.4 degrees Fahrenheit may increase metabolic demands of the body, often making exercise more difficult. Thus, many authorities recommend starting with lighter levels of exercise with a fever, and using overall performance to advancing to higher intensity of exercise. Some athletes may perform quite adequately with a fever, while others will need complete rest from exercise until the fever is gone for at least 24 hours.
I have found that the neck rule can also assist athletes and parents in deciding on sport participation, with or without a fever:
- If symptoms are entirely above the neck (runny nose, sore throat, mild headache, etc) then there is less potential risk for more serious illness with exercise. Recommend light exercise at first, and if symptoms do not worsen, then gradually increasing the intensity of the exercise.
- If symptoms are below the neck (productive cough with mucous, chest pain/tightness, stomach ache, vomiting/diarrhea, rash, muscle/body aches) then there is a greater risk not only for worsening individual symptoms, but also for spread to teammates. Thus, recommend no activity until these symptoms are gone for 24 hours. If there is any concern contact your medical provider to receive further evaluation.
How can we limit spread of colds and other illnesses during the winter months?
Multiple factors contribute to healthy function of the immune system in preventing illness
No athlete wants to be sick during the season and no athlete wants to spread illness to other team members. Following some basic rules can help prevent the spread of infections:
- Do not share water bottles, cups, towels, washcloths, or tissues.
- Shower immediately after exercise and change into clean clothes.
- Launder athletic equipment on a regular basis.
- If prescribed medications- take them as directed for the full length of the prescription.
- Use antibiotics only for the intended illness; never use them for a new illness or when they were not specifically prescribed. Incomplete or improper use of antibiotics can lead to bacterial resistance that may increase both the spread and severity of an illness.
- Get adequate sleep and nutrition as fatigue and poor diets can weaken the immune system. Get no fewer than 8 hours of sleep a night, and schedule at least one rest day from exercise per week. Low-fat diets (less than 10-15% of daily calories as fat) and less than 4-5 fruits/vegetables per day can also reduce ability to fight infection.
- Consider the Influenza Vaccine (flu shot) in the fall months. Influenza A/B viruses are common sources of illness and disability during the winter months and flu shots can reduce both individual and team risks from flu symptoms.
How does the amount of exercise influence risk of getting sick?
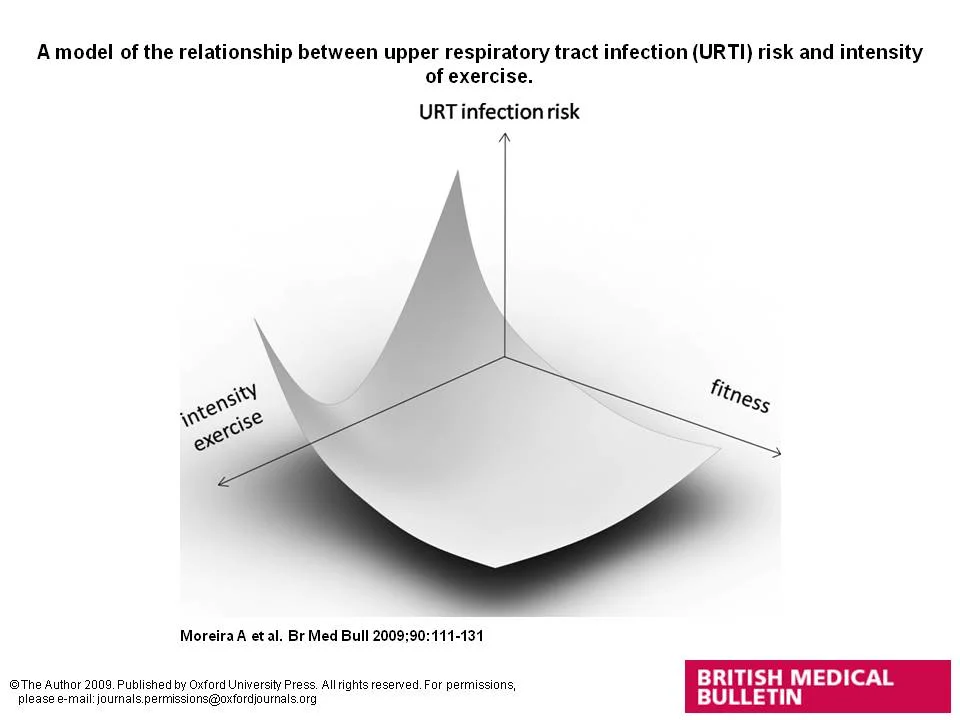
Moreira A et al. Br Med Bull 2009;90:111-131, © The Author 2009. Published by Oxford University Press. All rights reserved. For permissions, please e-mail: journals.permissions@oxfordjournals.org
The above figure demonstrates that both intensity of exercise and fitness level can influence the risk of upper respiratory infection. More moderate levels of exercise can be protective against illness, while lower levels and higher levels of exercise may actually be related to an increased risk. This is often why athletes get sick right after higher level competitions or at the end of a particular sport season. Higher levels of fitness may also be protective against respiratory illnesses.