Elite level volleyball tends to attract taller players who happen to have longer arms and fingers more conducive to blocking and hitting. Those same characteristics that provide a competitive advantage on the court may also unfortunately be a marker for a condition called Marfan Syndrome which has abnormalities in the connective tissue of the body leading to dilation (widening) of the aorta.
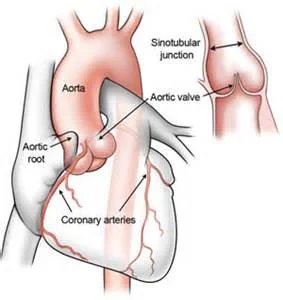
The aorta is the tube-like vessel that transports blood flow from the left side of the heart to the rest of the body. Widening of the initial segment of the aorta (known as the root and ascending aorta) can take place by itself and can also be found in cases of connective tissue disorders (like Marfan syndrome). A wider aorta may lead to higher risk of rupture (dissection) leading to sudden collapse and most often death.
So when working with a group where everyone is tall and thin, is there sufficient information to help us determine individual player risk and proper modes of evaluation?
While it might be logical to think that taller people should have wider aortic measurements, there has been a lack of data determining normal versus potentially abnormal and even dangerous measurements in tall athletes. One study of Italian Olympic Athletes proposed aortic root measurements greater than 4 centimeters in males and 3.4 centimeters in women might be worrisome, but only a few volleyball players were included in this study.
Thus, I am so very proud to share the article Cardiovascular and Musculoskeletal Assessment of Elite US Volleyball Players that was published by trusted USA Volleyball cardiology specialty colleague Paul Grossfeld and his associates at Rady Children's Hospital in San Diego.
Paul's study attempted to fill a knowledge void by evaluating elite US Volleyball players using:
- medical and family histories
- targeted physical examinations specifically focusing on abnormalities present in Marfan syndrome
- transthoracic echocardiograms.
What was found in the 37 male and 33 female US National Team members?
- Three male athletes (8%) had an aortic sinus diameter greater than or equal to 4 cm, one of whom also had an ascending aorta greater than 4 cm.
- Two female athletes (6%) had aortic sinus diameter greater than or equal to 3.4 cm, and another had an ascending aorta of 3.4 cm.
- There were no other intracardiac or arterial abnormalities.
- Individual musculoskeletal characteristics of Marfan Syndrome were common among the athletes but not more frequent or numerous in those with aortic dilation.
Paul and his colleagues concluded that the prevalence of aortic root dilation in this population of athletes was higher than what has previously been reported in other similar populations. He also recommended long-term follow-up of these athletes as essential to better determine the potential contribution of high-level volleyball training versus individual aorta characteristics as the cause of the aortic dilation to better identify the risk of further dilation and dissection.
These findings and recommendations apply most directly to adult, elite volleyball players, but should be of interest to a wider population that includes younger volleyball players, non-elite adult volleyball players, and other taller, thinner elite athlete groups such as basketball players, crew rowers, and track and field jumpers.
Perhaps future efforts will provide more specific screening and evaluation recommendations for a wider group of volleyball players, namely junior level/collegiate athletes and non-elite level adults.
Very grateful to Paul and his group for his diligence and insight, and eager to have the opportunity to share our expanding volleyball medicine knowledge with the entire volleyball community.