Seven Practical Observations on Dealing with Shin Pain in Athletes
After seeing plenty of shin pain in ballet Nutcracker performers , Olympic Volleyball players and various other athletic activities , here are 7 practical clinical observations to help assess and treat this common problem.
1) Look above the shin
Landing from a jump with inadequate hip or buttock strength can lead to an inward collapse of the knee, placing abnormal rotational forces on the shin. Similar lack of upper leg control can lead to collapse of the foot arch in running, again causing increased stress on the shin. Any complete evaluation of shin pain should include some form of hip/buttock strength- my favorites include the single-leg squat, step-ups,or plie in 2nd position for dancers. Ideal alignment has kneecap directly under the hip and over the 2nd toe.
Plie in second position: note kneecap directly under hip and over 2nd toe
2) Look immediately below the shin
Decreased ankle dorsiflexion (ability to move shin towards the foot or foot toward the shin)is yet another contributor to increased stress of the shin bones. Common causes include tight calf muscles or restricted movements between the tibia (shin bone) and the talus (first bone of the foot). Side-to-side dorsiflexion motion comparisons can help identify abnormalities.
3) Try to stand on toes or walk on the outside of the foot
If the calcaenous (heel bone) doesn’t move inward when standing on the toes, or if there is an inability to walk comfortably on the outside border of the foot, start thinking about restricted midfoot subtalar joint motion. Much like limited dorsiflexion, subtalar dysfunction transmits excessive forces to the shin region. Tarsal coalition is a fairly common and under-recognized form of subtalar restriction.
4) Never under appreciate the importance of the big toe
Amazing how restrictions within the small 1st metatarsophalangeal joint (aka big toe joint) can lead to big problems in the shin. Limited ability to raise the big toe off the ground toward the shin leads to either increased pressure on the outside of the foot or higher forces on the front of the shin during foot impact with the ground. Stretching of the flexor hallicus longus muscle that controls big toe motion can be life and career-saving.
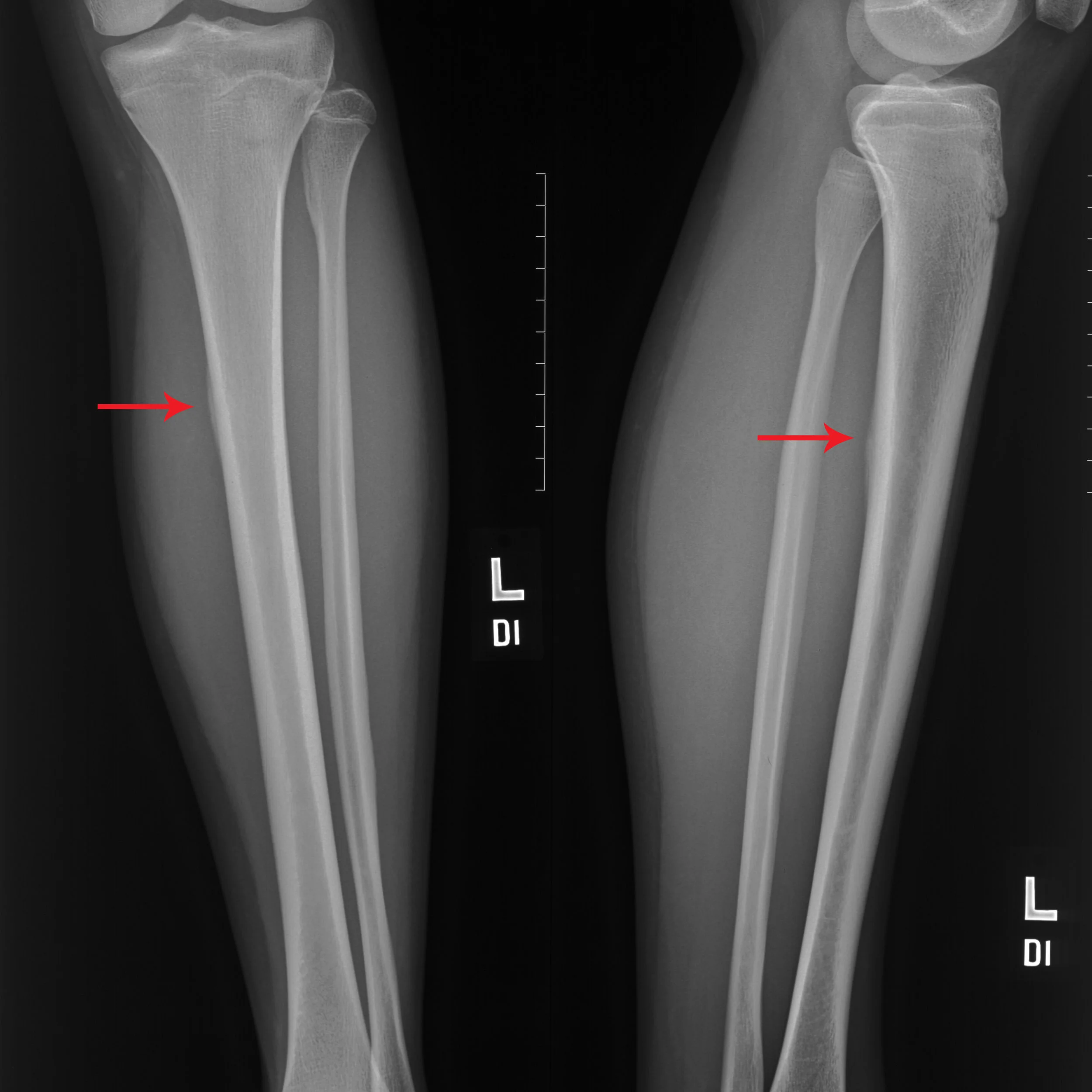
5) Stressful causes of cramping calves
While most forms of generalized tightness or cramping in the calves are usually due to muscle fatigue and relative overuse, be more suspicious of cramps that can be pointed out by a finger tip and are located right next to the upper part of the tibia bone. Have found 2 recent cases of tibial stress reactions that presented with the primary concern of localized calf cramps.
6) How are the iron stores?
Some cases of long-standing or difficult to treat shin pain may be complicated by low ferritin (measure of iron stores in the body). More likely in females with heavier menstrual losses or those athletes and performers with restricted dietary iron intake. I will routinely order laboratory testing in my evaluation of challenging shin pain.
7) What are you wearing on your feet?
source:http://runhealthylifestyle.com/2016/08/25/careful-flip-flops-dangerous-summer-choice/
Practicing in Southern California, I often see patients who will select the best in athletic footwear, but then come into my office and routinely report wearing ill-fitting or poorly supportive shoes or sandals for non-athletic activities. I’ve learned that if you can twist a shoe or sandal like a rolled newspaper, then there isn’t much mid-foot support. Use of relatively inexpensive over-the-counter arch supports in daily use shoes can allow one to be both fashionable and functional, while leaving sandals for the pool or beach.