1. Have you noticed any different approaches that you need to take throughout treatment of dancers who have or might have anorexia nervosa?
For all patients dealing with anorexia nervosa, one of the main initial issues is acknowledgingthat they suffer from the illness. Given that many dancers have a high sense of self-identity with their dance work, it can be even more challenging to come to this initial stage of acceptance. There is a fear not being able to dance, which then leads to a fear of not being identified as a dancer, and then ultimately a collapse of how they view themselves. In approaching treatment recommendations, one has to focus on the eventual performance enhancement goals, such as becoming a stronger, healthier, and more confident dancer.
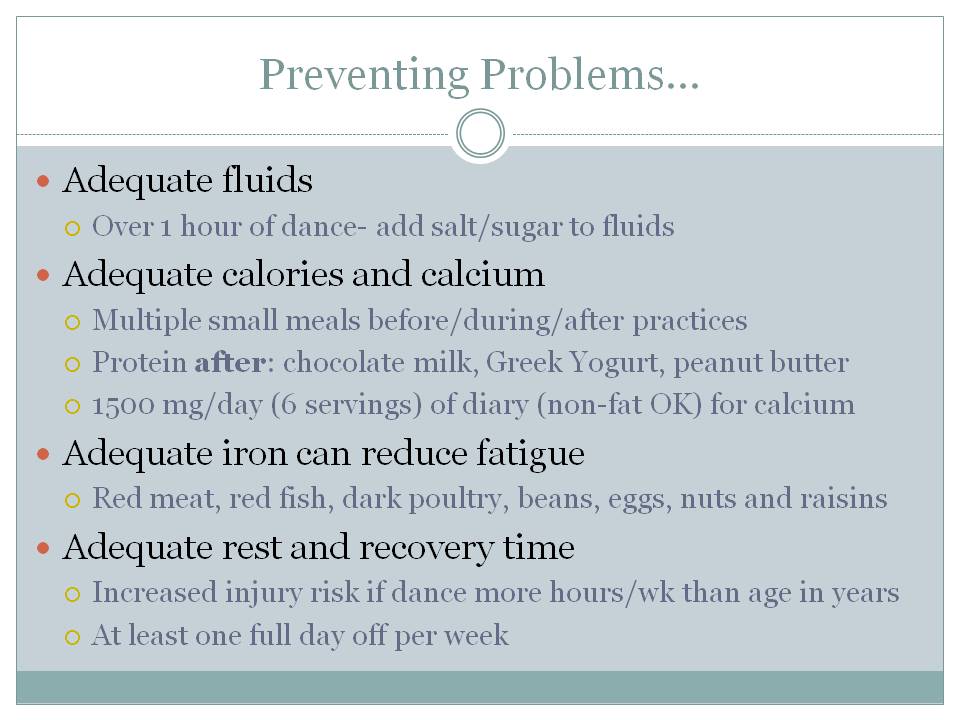
Dancers often deal from a particular sub-type termed “exercise anorexia” where there is insufficient caloric intake to match often excessive exercise energy demands. This might occur in part due to ignorance of the nearly 4,000-5,000 calories that can be burned a day by intense dance, or the energy defiency could also be intentionally created by dancers who do additional exercise (treadmill, stair machines, elliptical above and beyond usual dance requirements. In working with dancers, I have learned to ask about the amount and frequency of exercise, both inside and outside the dance studio. This extra exercise may represent a compulsive behavior that is a direct part of the anorexia nervosa illness.
Many young dancers have limited financial resources which often means making compromises on the amount or type of food intake. I often see reduced intake diary and meat products, which are high calorie food sources that also have calcium and iron.
Female dancers often report higher levels of caffeine, nicotine or even illicit cocaine use both for stimulating energy levels and appetite suppression.
In dealing with dancers, one must address these more common dance world issues to provide individualized and comprehensive care. Initially, a dancer may deny any problems with food intake, excessive exercise, or substance use, but as rapport and comfort are built with the medical team, such concerns may be more readily shared.
I also try to link the energy intake issues with the increased risk for bone stress injuries/fractures and irregular menstrual periods (in females) to educate the dancers and underscore the importance of appropriate medical care for the long-term health of a dancer’s career.
One helpfulthing about dancers is that they are used to working with multiple team members, from fellow dancers to multiple choreographers and instructors. Thus, once they understand that optimal treatment of anorexia nervosa requires an inter-disciplinary approach including physicians, nutritionists, and mental health providers, a dancer is more apt to accept this team-based treatment approach.
Dancers are used to tight, goal-oriented schedules, so I have found that setting short-term realistic goals definitely help in building confidence and compliance. Regular visits to modify goals and constant communication between providers (with appropriate privacy safeguards, of course) are also quite helpful.
2. In your experience, what affect does the dance world and its aesthetic standards have on dancers?
The aesthetic standards of the dance world favor lean physiques- from body revealing costumes and clothing to the demands of jumping, leaping, and partnering. Every day in the studio, a dancer is bombarded by direct comparisons with fellow performers in a competitive environment with occasional added subtle, or not so subtle comments (“you’d jump better if you were 5 pounds lighter”).
In some ways, the decisions behind anorexia give a dancera sense of control in an environment where there are constant uncertainties, such as being selected for a troupe, cast for a particular role, having to wear certain costumes, or being able to meet the demands of the choreographer.
With initial weight loss, many dancers gain a boost of confidence with increased jumping and turning abilities, and may hear approval and confirmation from colleagues and instructors. This definitely makes acknowledging early issues with energy intake more difficult, and often medical care is sought only when there is a later significant decrease in performance.
3. Have you seen more incidences in boys or girls and why do you think that is?
Studies definitely indicate a higher incidence of anorexia nervosa in females, which in the dance world is likely due to expectations such as costume choices, subjective ideals about form and technique with leaping and jumping, and ease of lifting lighter dancers when partnering.
However, one should not underestimate the incidence of anorexia in male dancers, who suffer similar demands on technique and form. While managing anorexia nervosa is a definite challenge in females, males actually have higher risk of more complicated outcomes, including death, from anorexia.
4. How do you feel that a patient's receptiveness to treatment would be affected if the medical professional they were working with had a background/previous understanding of dance?
I think that dancers will definitely be more receptive to working with medical professionals that know the culture of the dance world and the expectations and demands placed on dancers. When a scared dancer hears that he/she is not the first dancer to seek treatment, and that a particular medical provider has indeed helped other dancers get healthy, they do not feel as isolated and are more likely to actively engage in a treatment plan.